
What is Vaginismus?
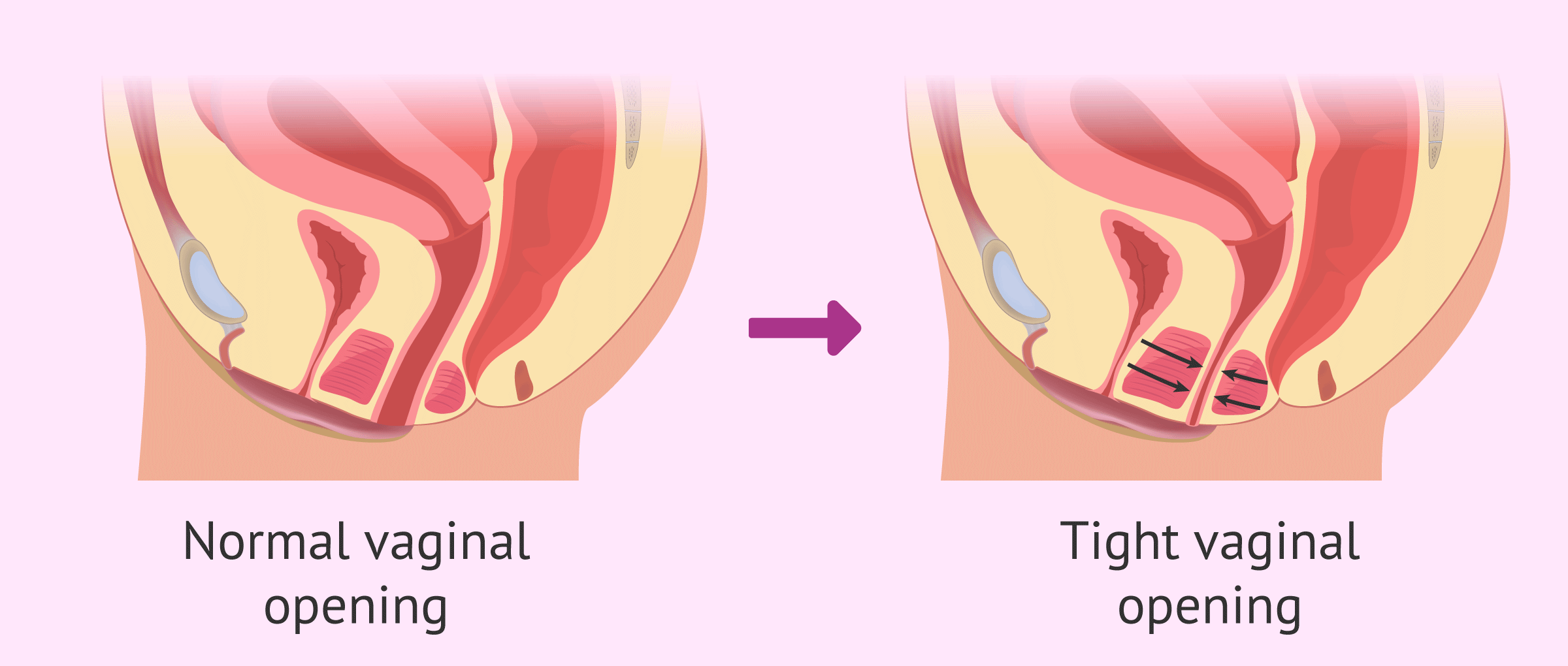
Vaginismus is an involuntary tightening of the pelvic floor muscles, making penetration painful or sometimes impossible. It is not simply “in the mind” — it is a reflex response that can be effectively managed with proper guidance and treatment.
Causes
Common causes include anxiety, past trauma, painful medical experiences, or lack of knowledge about the pelvic floor. Sometimes, no clear cause is identified — but that does not mean it cannot be treated.
How to know if I Have Vaginismus?
When asking yourself, “Do I have vaginismus?” it’s important to pay attention to how both your body and mind respond in situations involving vaginal penetration. The following signs are common indicators — especially if you experience more than one:
1. Difficulty inserting a tampon
For many women with vaginismus, inserting a tampon feels nearly impossible. It may seem as though the tampon is “hitting a wall.” Even with effort, it won’t go in comfortably, and repeated attempts can lead to pain or even more muscle resistance.
2. Anxiety about penetration
If the thought of penetration makes you feel tense, fearful, or anxious, vaginismus may be the underlying reason. This anxiety can be linked to past trauma, negative experiences, or lack of confidence with intimacy. Over time, the cycle of fear and avoidance can also affect self-esteem and emotional wellbeing.
3. Involuntary pelvic floor spasms
One of the hallmark signs of vaginismus is the involuntary tightening of the vaginal muscles. These spasms are often painful and beyond your conscious control. In some cases, the pelvic floor remains in a constant state of tightness, known as a “hypertonic pelvic floor.” This can also cause constipation, urinary urgency, pelvic discomfort, and tension in nearby muscles such as the hips or lower back.
4. Painful or impossible intercourse
Because of the muscle contractions and spasms, sexual intercourse may feel extremely painful or unachievable. Some women can still experience arousal and orgasm through clitoral stimulation, but penetration remains difficult or impossible. For others, anxiety about penetration may even prevent arousal altogether.
5. Difficult gynecological exams
Routine gynecological exams can be especially challenging. For women with vaginismus, attempts to insert a finger, tampon, or medical instrument such as a speculum may cause sharp, burning, or stinging pain. In some cases, examinations cannot be completed due to the involuntary muscle response.
Types of Vaginismus
Though symptoms are similar, vaginismus is usually classified into two main types:
- Primary vaginismus — present from the very first attempt at penetration. Women may find it impossible to use tampons or undergo their first gynecological exam.
- Secondary vaginismus — develops later after a period of pain-free penetration, often linked to trauma, childbirth, surgery, or emotional stress.
Surgery is the only solution? No!
In almost all cases, surgery and medication is not a must. Vaginismus usually responds well to non-invasive care. The most effective approach combines physiotherapy techniques, education, and gradual training of the pelvic floor muscles.
Breathing and Relaxation Techniques
- Essential part of vaginismus treatment.
- Deep diaphragmatic breathing, mindfulness, and relaxation exercises calm the nervous system and reduce involuntary tightening.
Use of Dilators
- Widely used in gradual desensitization programs.
- Allow the vaginal muscles to adapt step by step, paired with relaxation.
- Best results when guided by a physiotherapist or sex therapist.
- Pick dilators that suit your progress. See our guide on choosing the right dilator.
Pelvic Health Physiotherapy
- The gold standard treatment for vaginismus.
- Integrates methods such as manual therapy, relaxation, education, biofeedback, and guided dilator training under professional supervision.
- Strongest evidence for long-term recovery.
⚠️Why Self-Training Can Be Risky
Attempting to treat vaginismus alone can lead to setbacks. Incorrect exercises, misuse of tools, or progressing too quickly may increase pain and reinforce fear. Professional supervision helps ensure safety, prevents relapse, and builds long-term confidence.
See our guide on how to select pelvic health centre wisely.